

The softball team was one of legendary success, often reaching the College Softball World Series. This particular preseason, two members of its starting lineup were each experiencing a chronic shoulder injury. The shortstop was battling a rotator cuff strain and the starting pitcher was struggling with anterior capsulitis. The two players were receiving care from two different athletic trainers, with two very different athletic training philosophies.
The athletic trainer responsible for developing the shortstop’s injury knew it was important to differentiate exactly which rotator cuff muscles were injured and specifically target those muscles—the infraspinatus and teres minor—through an individualized rehabilitation plan. The plan was a success and the healthy shortstop had a great season, even earning All-American honors.
Unfortunately, the same was not true for the pitcher. She had shoulder surgery prior to preseason, with the intent to rehabilitate the shoulder and be ready to start the season. However, the athletic trainer in charge of her rehabilitation plan did not address the specific anatomy involved and approached it as “any other shoulder injury,” utilizing the same rehabilitation plan that was created for the shortstop. The pitcher’s shoulder condition worsened over the preseason and, ultimately, she never pitched again. This tragic example of a rehabilitation plan gone badly (very badly) is an important reminder of just how critical it is for the clinician to have a thorough understanding of anatomy. So let this story sit in the back of your mind any time you are tempted to use a cookie-cutter rehabilitation protocol. Remember that each patient is an individual and deserves a plan designed just for them and their injury.
Based on your own observations and knowledge, think about the questions below. What can you guess at or hypothesize? You can test your answers as you read and when we revisit the questions at the end of the chapter.
biomechanics
bursa
bursitis
congruency
frontal plane
kinetic chain
mechanism of injury
mechanoreceptors
oblique plane
pathology
proprioception
sagittal plane
scapulohumeral rhythm
separated shoulder
transverse plane
winging of the scapula
For many students, learning the shoulder complex can seem overwhelming at first, as it is, indeed, rather complex. This chapter takes you through the shoulder region joint by joint, to help you better understand its complexity.
A useful approach for learning the inner workings of the shoulder complex—and its relationships to other regions of the body—is to look at it as a puzzle (2.1).
For example, when we identify an injury to the glenohumeral joint (the true shoulder joint), is it a primary injury? Or is it a secondary injury as a result of a deficiency somewhere else within the shoulder complex or in the lower kinetic chain and/or core? Why would we even need to consider these areas? Because they, too, can be key pieces in the puzzle.
A body’s kinetic chain is made up of interrelated links or segments—such as muscles and joints—that follow a predictable movement pattern. Movement of one segment affects movement patterns at one or more other segments.
Many shoulder injuries in throwers are due to poor biomechanics, or how forces affect the body. But these poor biomechanics are not only within the shoulder complex. When someone throws a ball, they use their entire body—the throwing motion begins at their toes and ends at their fingertips. The thrower is utilizing the entire human kinetic chain. Thus, a biomechanical deficiency or injury anywhere along that chain may impact the function of the shoulder complex. For instance, a softball player with turf toe will have trouble bearing weight on the injured foot, which potentially impacts their throwing mechanics. It all comes back to how the pieces of the puzzle fit together.
The first step in putting together a puzzle is to separate the edge pieces and begin building the framework of the puzzle. We can do the same thing with the shoulder complex (2.2); we can begin by identifying the various joints (articulations) within the shoulder complex. This will be our framework.
2.2 A 3D view of the shoulder complex
There are three true articulations and two false articulations (2.3, 2.4). A true articulation is one in which the bones are in contact with one another, which means they have some level of congruency. A false articulation is one in which the bones do not actually come into contact with one another, but their relationship to one another is no less important.
True Articulations
Sternoclavicular (S/C) joint
Acromioclavicular (A/C) joint
Glenohumeral (G/H) joint
False Articulations
Scapulothoracic (S/T) joint
Coracoclavicular (C/C) joint (coracoclavicular ligament)
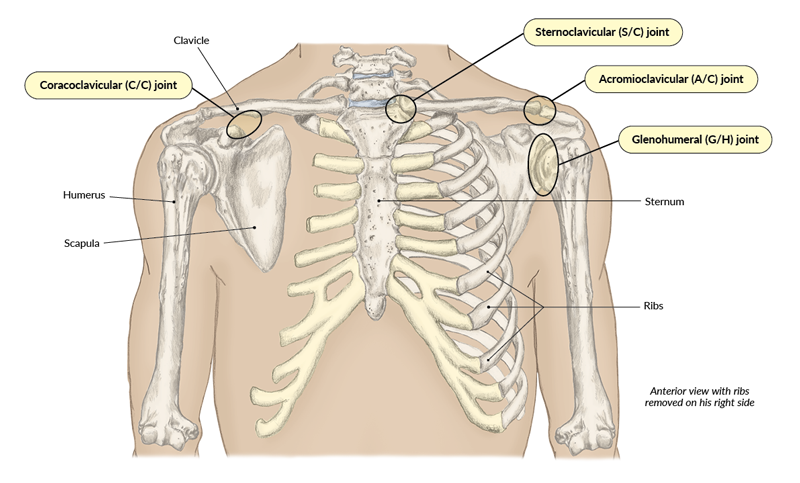
2.3 Anterior view of joints of the shoulder complex
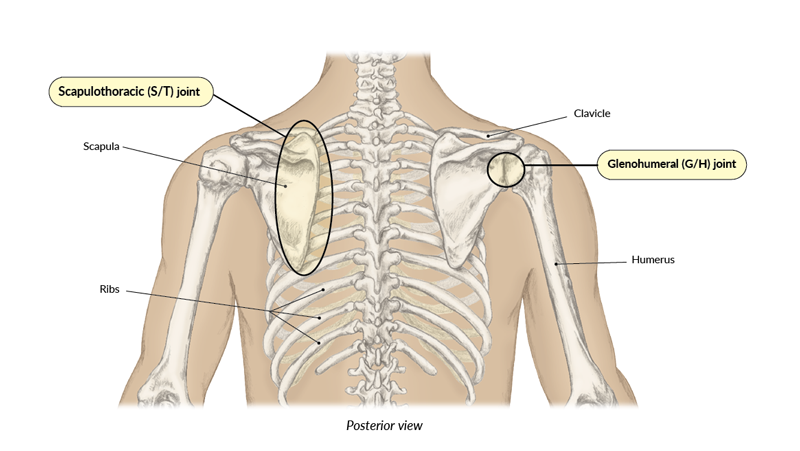
2.4 Posterior view of joints of the shoulder complex
Once we have the framework established, we can begin filling in the puzzle of the shoulder complex by identifying the functional anatomy of the supporting tissues of each articulation, whether true or false (the type of joint, not a question!).
The shoulder complex is a commonly injured area of the body—particularly in individuals who participate in overhead activities such as throwing, swimming, and gymnastics. For example:
To achieve a proper high five (and make your bestie smile), the shoulder complex will produce multiple actions. In fact, the shoulder complex has many motions that occur within it. Among the various joints of the shoulder complex, movement can occur in the following planes: sagittal, transverse, frontal (or coronal), and oblique. As we perform our daily activities throughout the day, or as a softball pitcher performs her skillset during practice, the shoulder complex is rarely moving in an isolated plane. Rather, two or more motions are likely occurring together. Adding to that complexity is scapular movement, which is critical for healthy mobility and proper function of the shoulder.
|
|
|---|
Plane of motion |
Movements |
|---|---|
|
Sagittal plane |
Extension |
|
Transverse plane |
Medial (internal) rotation |
|
Frontal plane |
Abduction |
|
Oblique plane |
Any combination of movements from the three primary planes |
Take a minute to review the motions of the shoulder complex (2.5, 2.6) and practice each movement as you are able.
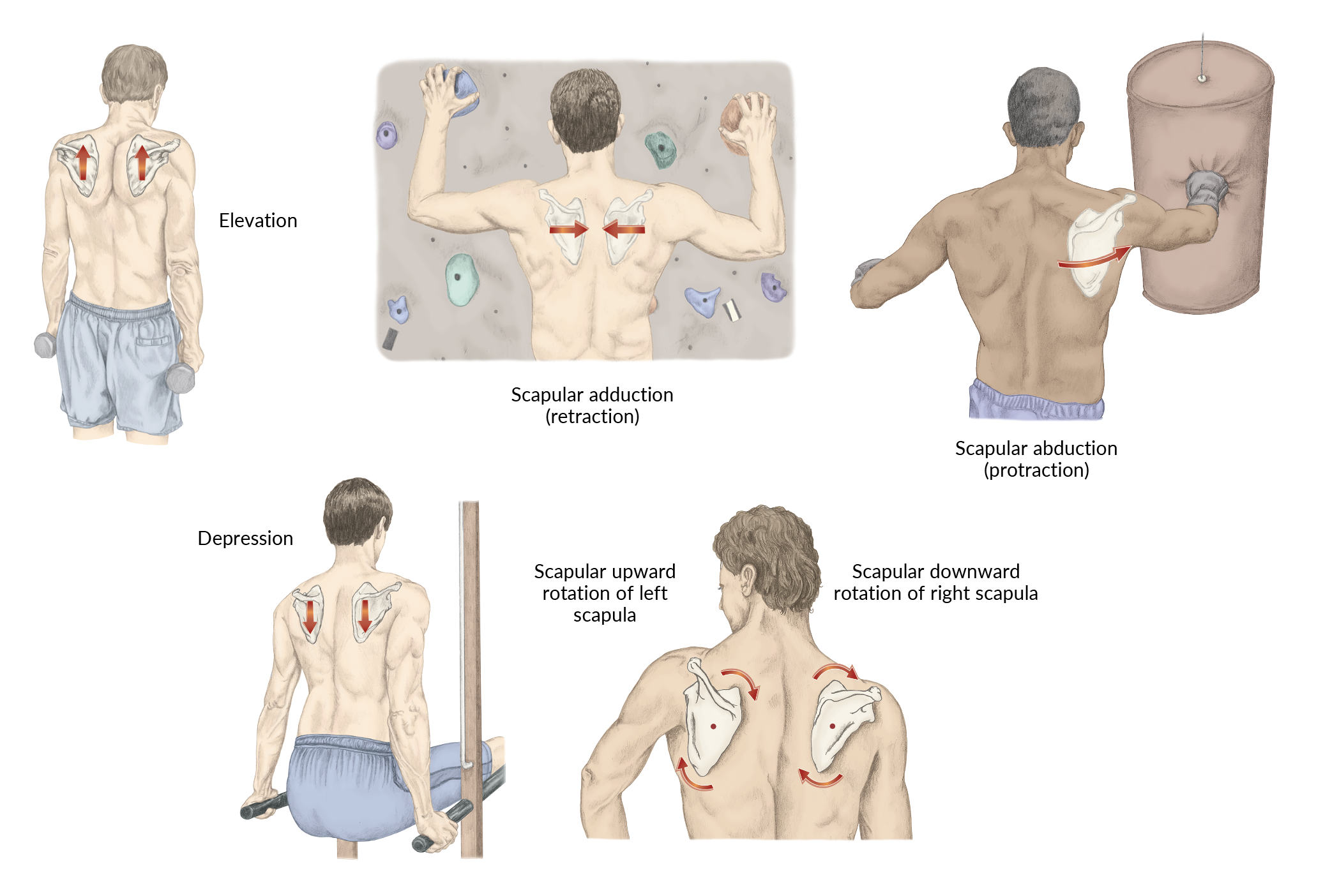
2.5 Movements of the scapula (scapulothoracic joint)
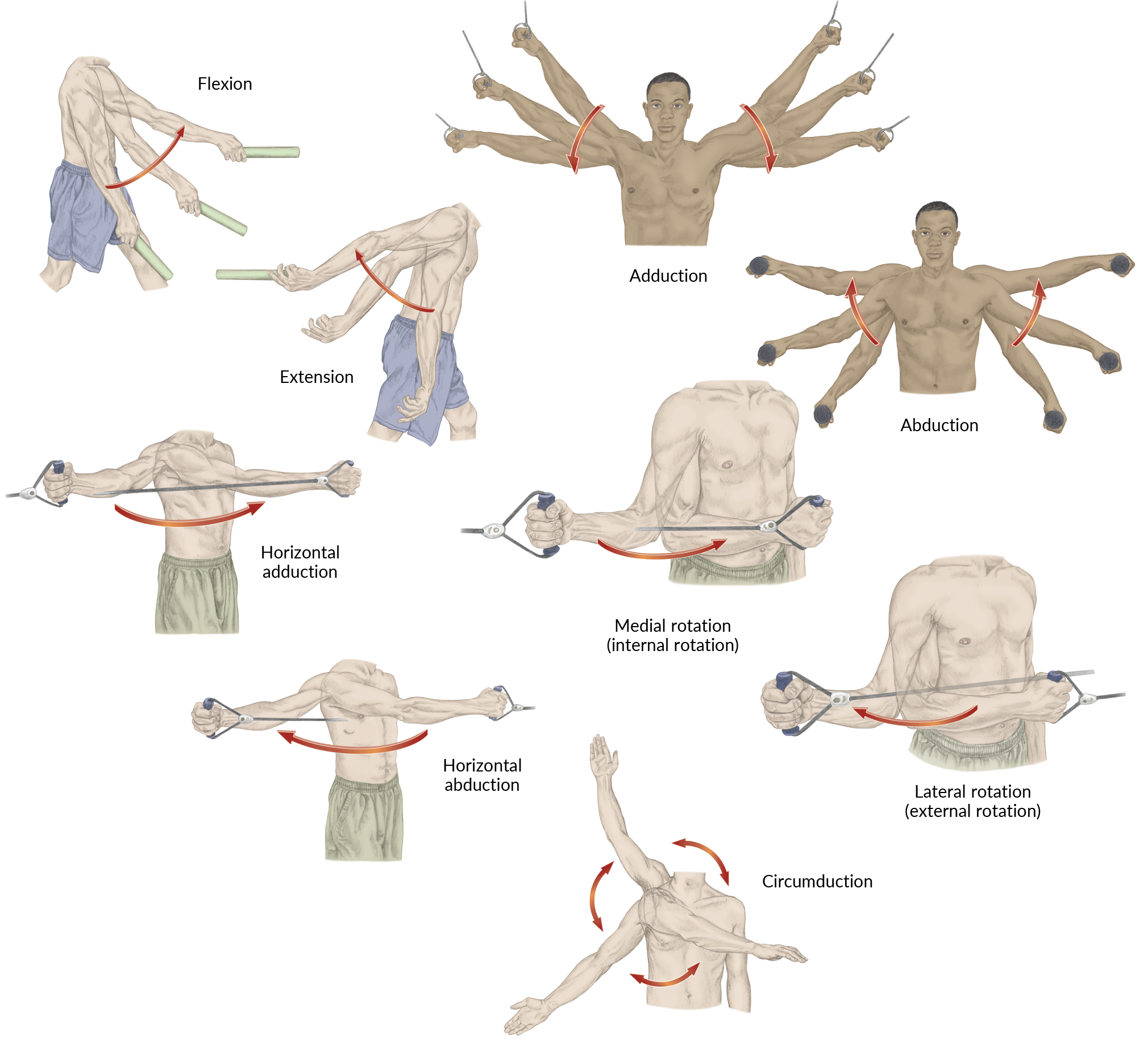
2.6 Movements of the shoulder (glenohumeral joint)
Give yourself a high five for your hard work learning anatomy. Now that your endorphins are elevated and you are energized, it is time to put the pieces of the shoulder complex together and solve the puzzle.

Before you proceed on your quest for knowledge of the joints of the shoulder complex, here are some questions to consider:
When building a framework, it is important to begin at the base or with the bottom edge of the puzzle. The sternoclavicular (S/C) joint is the bedrock of the shoulder complex. While it is quite stable—you will soon learn why—it is impacted by every movement of any of the shoulder joints, whether they are true or false. Let us take a deeper look at its functional anatomy.
The sternoclavicular joint is a synovial, saddle-shaped joint that consists of two bones, the sternum and the clavicle (2.7). More specifically, the medial/sternal end of the clavicle articulates with the manubrium. The name of this articulation is deceiving because the clavicle also ever-so-slightly articulates with the first rib. But the congruency between the clavicle and the sternum affords the joint much stability.
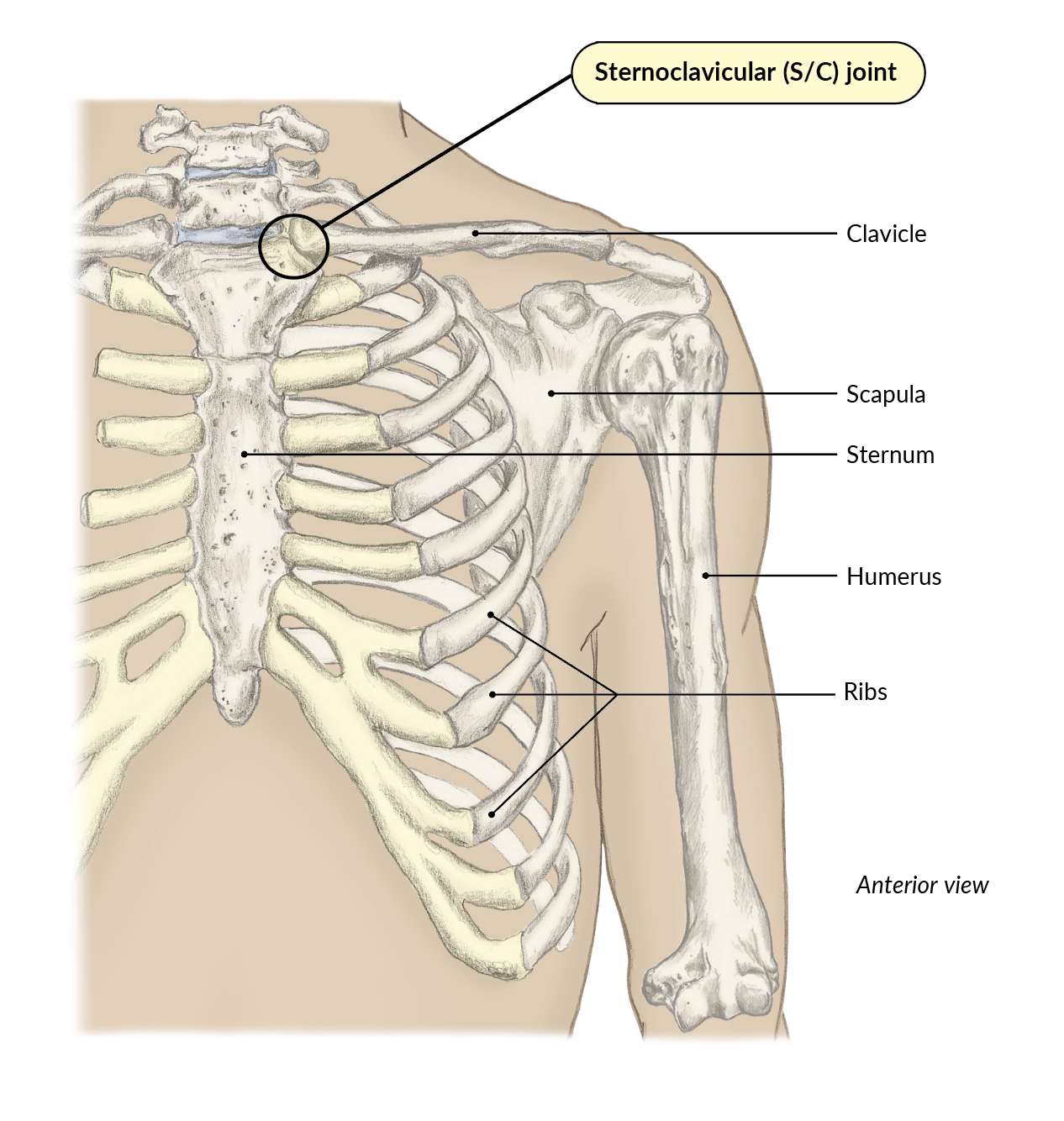
2.7 The sternoclavicular (S/C) joint
While little movement actually occurs at the S/C joint, there is slight movement within the articulation during scapular elevation, depression, adduction (retraction), and abduction (protraction).
You can put this into action. To get a feel for the movement at this articulation, place the tips of the index and middle fingers of your right hand over your left S/C joint. Now raise your left arm into shoulder abduction. Now try forward flexion of the shoulder. Lastly, try horizontal abduction. Do you notice that whichever way you move your shoulder, your S/C joint fluctuates slightly? This is true for movement in all directions: shoulder flexion, extension, abduction, adduction, medial (internal) rotation, lateral (external) rotation, horizontal abduction and adduction, and circumduction.
Imagine having an injury to the S/C joint—it would be rather debilitating. (You would have a hard time high-fiving your friends!) Even breathing may be painful with an S/C joint injury. This seemingly simple articulation plays a big role in the shoulder complex.
The stability of the S/C joint is further strengthened by a fibrocartilaginous articular disc (2.8). The articulation is also supported by the anterior sternoclavicular (S/C) ligament (2.8) and the posterior sternoclavicular (S/C) ligament (not shown).
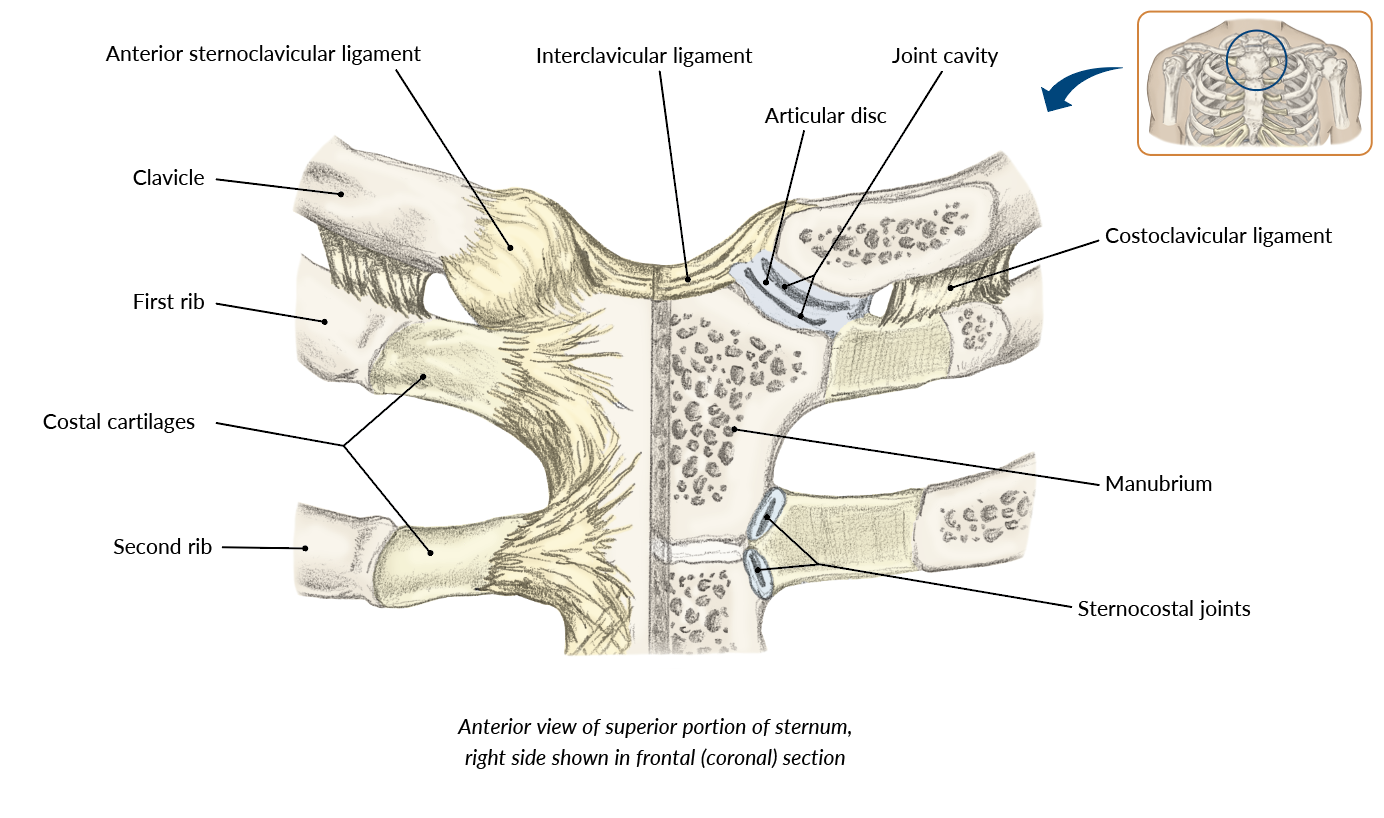
2.8 Connective tissues supporting the sternoclavicular joint
One compelling example of the sternoclavicular joint’s clinical relevance in the human body is that if the S/C joint suffers a dislocation, our hope would be that it is an anterior dislocation versus a posterior dislocation. While dislocations are rare to the S/C joint (only 3% of all shoulder dislocations[1]), a posterior dislocation could have a devastating impact on the ability to breathe and swallow. If the clavicle is forced posteriorly, it could penetrate the trachea. This is rare but deadly serious—a true medical emergency. Thankfully, anterior dislocations are much more common (nine times as common) compared to posterior dislocations (2.9).[2]
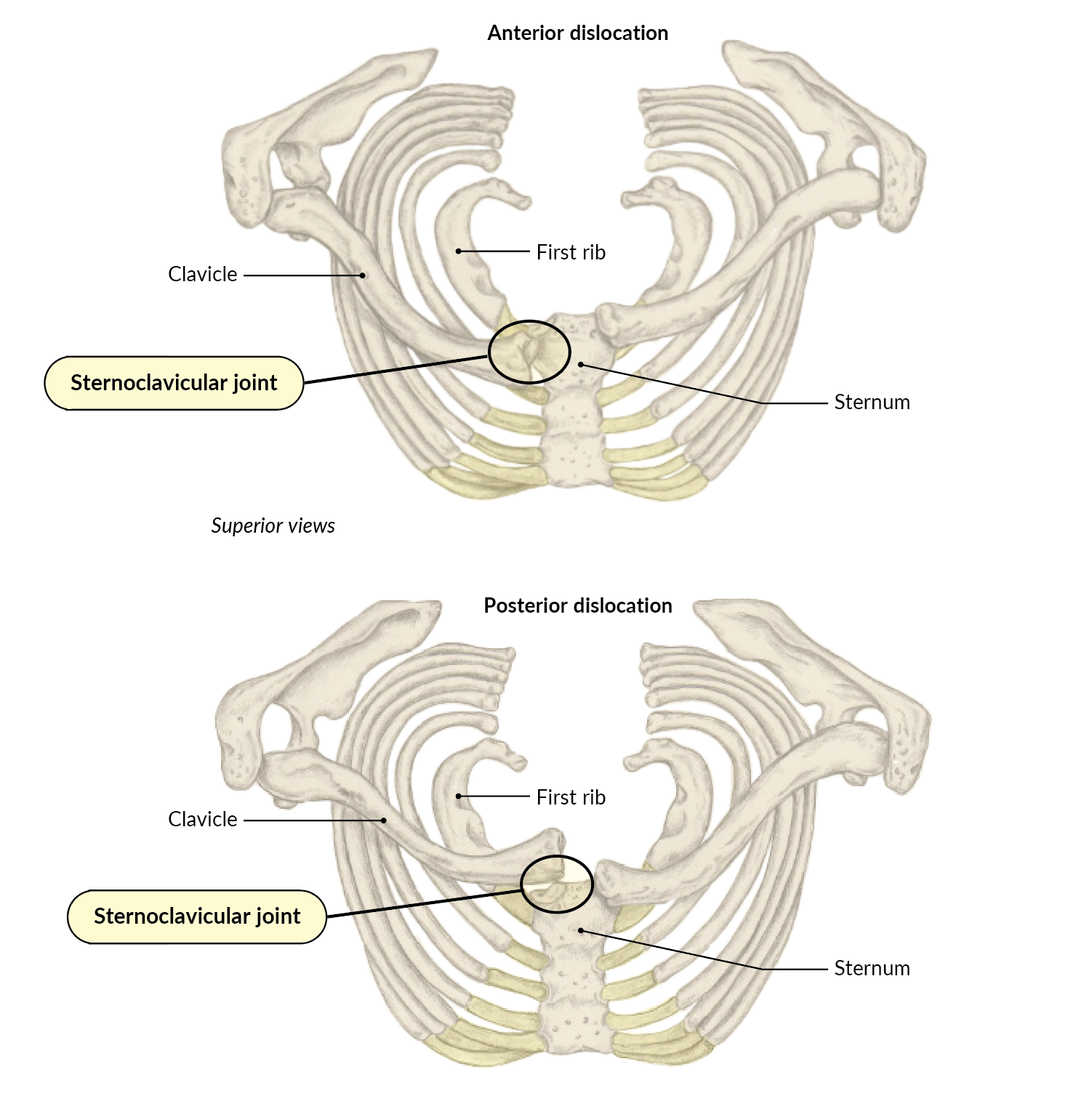
2.9 Anterior and posterior dislocations of the sternoclavicular joint
The Sternoclavicular Joint
Use this quiz to review what you have learned
The acromioclavicular (A/C) joint is another example of a stable articulation that depends upon skeletal congruency—in this case, between the acromion and the lateral/acromial end of the clavicle (2.10).

2.10 The acromioclavicular (A/C) joint
The acromioclavicular joint is a synovial joint where very little motion occurs, as it allows for only a gliding movement. Because it attaches the scapula to the clavicle, the A/C joint helps to facilitate shoulder abduction and flexion (2.11). It also assists in transmitting forces from the upper extremity to the axial skeleton.
HD, HD web
2.11 The A/C joint facilitating shoulder abduction and flexion when lifting weights
The A/C joint is primarily supported by the acromioclavicular (A/C) ligament, which prevents the clavicle from “separating” from the acromion. The articulation is further supported by the coracoclavicular and coracoacromial ligaments. The coracoclavicular ligament assists the A/C ligament in maintaining the proper position of the clavicle. The ligament originates from the coracoid process and inserts onto the clavicle, where it splits into two smaller ligaments: conoid and trapezoid (2.12).

2.12 Ligaments supporting the acromioclavicular joint
The coracoacromial ligament provides secondary support to the A/C joint as it originates from the coracoid process and inserts into the acromion. While it may seem that this ligament would not play a significant role in the shoulder complex, its integrity is important to the static stability of the shoulder; it aids in load distribution across the acromion and prevents displacement of the humeral head.
Additionally, the coracoacromial ligament provides dynamic stability for the shoulder complex to maintain proper biomechanics and proprioception, or the awareness of the body in space. This unassuming ligament has a direct impact on proprioception throughout the movements of the shoulder because of the mechanoreceptors located within it. Mechanoreceptors are sensory receptors that detect changes in tension, pressure, stretch, and motion.
We have talked about injuries to a softball shortstop and a pitcher. Now is a good time to include another example—a true story about the third baseman on the same team. While making a play on a routine hit up the third baseline, the player fielded the ball and began their throwing motion toward first base. Unfortunately, the cleats on the right shoe became entangled in the shoelaces of the left, causing them to trip and fall. They landed on the tip of their adducted shoulder—a classic cause, or mechanism of injury, for a separation of the clavicle away from the acromion, commonly called a separated shoulder. (With all these injuries, it is even more impressive that this softball team returned to the College World Series!) This type of fall (2.13) could also cause the ligaments that support the A/C joint to stretch (a sprain) or tear, particularly the A/C ligament.

2.13 Landing on an adducted shoulder can injure the A/C joint.
The Acromioclavicular Joint
Use this quiz to review what you have learned
When most people refer to the shoulder joint, they are actually referring to the glenohumeral (G/H) joint. But how does this articulation fit into our puzzle theme? Think of the glenohumeral joint as the center of the puzzle, the part that all of the other pieces surround and connect to. The G/H joint is the pivot point of the shoulder complex.
The glenohumeral joint consists of two bones, the humerus and the scapula (2.14). More specifically, the head of the humerus articulates with the glenoid cavity (also called the glenoid fossa) (2.15, 2.16). The head of the humerus is round and convex; the glenoid cavity is a shallow, concave structure.

2.14 The glenohumeral (G/H) joint, or true shoulder joint
 2.15 The head of the humerus and the glenoid cavity
2.15 The head of the humerus and the glenoid cavity
 2.16 The glenoid cavity
2.16 The glenoid cavity
So, we have a round object (head of the humerus) rolling across an almost flat surface (glenoid cavity) with any movement of the glenohumeral joint. Think of a ball sliding across a slightly cupped hand or a golf ball sitting atop a tee (2.17). In each case, the ball has very limited contact with the hand or tee. Similarly, the G/H joint has limited congruency between the articular surfaces of the bones.

2.17 Like a golf ball on a tee, the bones of the G/H joint have limited congruency.
This ball-and-socket joint structure is well designed for mobility but provides very limited skeletal support. More simply put, it gives up stability for mobility—a phrase you have likely heard. As you think back to the softball shortstop and pitcher, this idea partially explains why they were both prone to injury.
The glenohumeral joint is where the obvious motion of the shoulder complex occurs (2.18): shoulder flexion, extension, lateral (external) rotation, medial (internal) rotation, abduction, adduction, horizontal abduction and adduction, and circumduction.
2.18 The glenohumeral joint in action during a game of table tennis
Because of the limited skeletal stability of the glenohumeral joint, it relies heavily on both static connective tissues (such as ligaments) and dynamic soft tissues (such as muscles and tendons) for its support and stability.
The primary static connective tissues are the following:
The glenoid labrum is an important puzzle piece for static support, as it brings much needed stability to the glenohumeral joint. This labrum is a fibrocartilaginous ring that is positioned around the perimeter of the glenoid cavity to provide greater depth to such a shallow anatomical structure (2.19). This increased depth protects the ball-shaped humeral head from sliding over the edges of the glenoid cavity when performing daily activities such as high-fiving your friend. Think of it as the fence that keeps the ball inside of the playing field.

2.19 The glenoid labrum
Three key ligaments assist in the static stabilization of the glenohumeral joint, particularly in preventing anterior dislocations. They are the superior, middle, and inferior glenohumeral ligaments (2.20). All three aid in stabilizing the glenoid cavity to the humeral head and creating the joint capsule.[3]
The superior glenohumeral ligament is an important stabilizer in the inferior direction. But it does not act alone. It works in conjunction with the coracohumeral ligament to achieve that stabilization. It also has a unique relationship with the long head of the biceps brachii, as they run parallel to one another. Specifically, the superior glenohumeral ligament runs from the anterior, proximal glenoid lip to the coracoid process.
The middle glenohumeral ligament originates from the neck of the scapula and the glenoid lip and inserts on the lesser tubercle of the humerus and the subscapularis tendon. It provides anterior stability for the glenohumeral joint between 45° and 60° of abduction.
The inferior glenohumeral ligament is the main stabilizer in preventing an anterior, inferior glenohumeral dislocation—a common shoulder injury. This ligament originates from the glenoid lip and inserts into the joint capsule wedged between the triceps brachii and subscapularis muscles.

2.20 The glenohumeral ligaments
Additionally, the glenohumeral joint is supported by ligaments adjacent to it, the coracoclavicular and coracohumeral ligaments (2.21). We have already discussed the coracoclavicular ligament. As a reminder, it plays a role in the static stabilization of the humerus, thus impacting the stability of the G/H joint.

2.21 The coracoclavicular and coracohumeral ligaments
The coracohumeral ligament has two functions in regard to its support of the G/H joint. The first function is rather expected and simplistic, providing stabilization at the proximal aspect of the glenohumeral joint capsule. The second function is to provide proximal stabilization of the long head of the biceps tendon within the bicipital groove (also called the intertubercular groove). This is possible because the ligament originates from the coracoid process and inserts into both the greater and lesser tubercles of the humerus. This small-but-mighty ligament may not always get a lot of attention, but it is essential to the health of the G/H joint and the long head of the biceps tendon.
Because the glenohumeral joint gives up stability for mobility, it requires muscles to provide dynamic support through the complexity of its motions.
Let us take a look at these various soft tissues and the significant roles they play in G/H joint stability:
A great place to start is with the rotator cuff muscles, or SITS muscles: Supraspinatus, Infraspinatus, Teres minor, and Subscapularis (2.22, 2.23). To review the origins and insertions of the rotator cuff (SITS) muscles, see Chapter 2 of Trail Guide to the Body.

2.22 Supraspinatus, infraspinatus, and teres minor
 2.23 Supraspinatus, infraspinatus, and subscapularis
2.23 Supraspinatus, infraspinatus, and subscapularis
For abduction of the shoulder, the deltoid is the primary mover and the supraspinatus is the synergist or the “wingman”—the muscle that does the initial work and sets the stage for success (2.24, 2.25). The supraspinatus is responsible for the first 15° of abduction. Then the deltoid takes over and brings the glenohumeral joint to 90° of abduction. This is what we refer to as true abduction. Beyond 90°, the upper trapezius and the serratus anterior bring the shoulder into full abduction. Full abduction is really a combination of abduction and medial (internal) rotation of the humerus working in conjunction with the scapula.
Another important fact about the supraspinatus: it is the most commonly torn of the SITS muscles, with tears occurring at a rate of 68.9% in males and 38.1% in females. Interestingly, supraspinatus tears are more common in older adults, males, smokers, diabetics, individuals with high blood pressure, and individuals with a critical shoulder angle (CSA).[4]
 2.24 Supraspinatus
2.24 Supraspinatus
2.25 A 3D view of the supraspinatus muscles
The infraspinatus (2.26, 2.27) and teres minor (2.28, 2.29) work together to create external rotation of the glenohumeral joint. Consider these muscles your workhorses. They play a significant role in overhead activities such as the overhand throw.

2.26 Infraspinatus
2.27 A 3D view of the infraspinatus muscles
 2.28 Teres minor
2.28 Teres minor
2.29 A 3D view of the teres minor muscles
Let us look at pitching, for example. These muscles are first concentrically active in the throwing motion. Their job is to pull the G/H joint into as much lateral (external) rotation as possible (2.30).

2.30 Infraspinatus and teres minor work together for lateral (external) rotation of the G/H joint.
A really cool thing about these workhorse muscles is that they also work eccentrically during the throwing motion. Their primary responsibility is to slow down the speed of the arm once the ball is released from the thrower’s hand (2.31).

2.31 Infraspinatus and teres minor slow down the speed of the arm once the ball is released.
This eccentric load occurs because the external load acting on the muscle exceeds the muscle’s force production at that moment in time. This results in a lengthening of the muscle and tendon. As you can imagine, this puts a great deal of stress on the infraspinatus and teres minor. Often, it is in this phase of the throwing mechanics that injury occurs to the lateral (external) rotators. So, you may be thinking, just do not put on the brakes; let the deceleration occur at its natural high-speed rate. But if that happened, the force of momentum would likely cause the pitcher to continue to spin past their follow-through—and fall over on the mound.
The subscapularis is the oddball of the SITS muscles, as it has a different insertion landmark than the other three. It inserts onto the lesser tubercle, whereas the other three SITS muscles insert onto the greater tubercle. Subscapularis is also a medial (internal) rotator of the glenohumeral joint. It is the largest and the strongest of the SITS muscles (2.32, 2.33).

2.32 Subscapularis
2.33 A 3D view of the subscapularis muscles
The subscapularis plays a role in preventing an anterior dislocation of the humerus. It contributes to adduction and, in certain positions, extension, providing even more of a dynamic support to the G/H joint. While the subscapularis is the least often injured of the SITS muscles, if it is injured, the injury is likely associated with an anterior dislocation.
The remaining structure related to dynamic stability of the glenohumeral joint is the long head of the biceps brachii tendon (2.34). The long head of the biceps brachii tendon is situated in the bicipital groove, located between the greater and lesser tubercles of the humerus.

2.34 The long head of the biceps brachii tendon
The bicipital groove has a roof—the transverse humeral ligament—to ensure the long head of the biceps brachii tendon stays within the groove. But it does not act alone, as it is assisted by the coracohumeral ligament.
In most everyday activities, the biceps brachii tendon does not play a significant role in the dynamic stability of the G/H joint. But as a clinician, you will evaluate, treat, and manage many injuries in patients who perform overhand activities such as throwing a softball or a javelin (2.35). The biceps brachii muscle specific to the long head tendon is very eccentrically active in throwing motion once the ball or javelin has been released from the throwing hand. As the elbow transitions into an extended position, a great deal of stress is placed upon the tendon. Ultimately, this could result in acute or chronic bicipital tendinitis.
2.35 Stress on the tendon during the act of throwing

Can you think of any predisposing factors that may lead to a rotator cuff tear?
Some examples:
Let us look at a common shoulder scenario. A shoulder dislocation is a very common injury, accounting for half of all types of major joint dislocations that occur annually.[5] What this actually refers to is a dislocation of the glenohumeral joint (2.36). And of those G/H joint dislocations, almost all of them are anterior as a result of forced lateral (external) rotation and abduction.
Posterior dislocations occur at a much lesser rate of just 2%–4% and inferior dislocations at an almost nonexistent rate (less than 1%).[6] Why, you may ask? The medial (internal) rotators of the glenohumeral joint are typically much stronger than the lateral (external) rotators; it takes a traumatic event to cause a posterior dislocation. For an inferior dislocation, it too takes a traumatic event to damage the inferior G/H joint capsule.

2.36 Anterior dislocation of the glenohumeral joint
The Glenohumeral Joint
Use this quiz to review what you have learned
The glenohumeral joint is the center of our puzzle because that is where the most obvious motion occurs within the shoulder complex. However, that motion would not be successful if not for the scapulothoracic (S/T) joint.
You may recall that the scapulothoracic joint is a false articulation. The unique design does not allow the bones of the joint, the scapula, and ribs 2–7 (or ribs 8 and 9 in some very tall people) to articulate. Therefore, the scapula has the ability to slide across the thoracic wall in a variety of movements, including abduction (protraction), adduction (retraction), elevation, depression, and rotation.
This mobility allows the G/H joint to reach (pun intended) its maximal range of motion in all directions. As the scapula moves, the position of the glenoid cavity in relation to the humeral head is affected. Thus, the relationship between the scapulothoracic and glenohumeral joints has to be a perfect fit, like that of puzzle pieces, for optimal biomechanics within the shoulder complex.
The S/T joint itself is more of a relationship that occurs between the scapula and the thoracic cage (2.37, 2.38, 2.39). The unique fit of these two “pieces” is critically important, not only for a biomechanically efficient glenohumeral joint, but also for the overall function within the shoulder complex. The scapula is a flat and irregularly shaped bone. Anteriorly, it has a concave surface that accommodates the convex nature of ribs 2–7.
 2.37 Anterior view of the scapulothoracic (S/T) joint
2.37 Anterior view of the scapulothoracic (S/T) joint
 2.38 Posterior view of the scapulothoracic (S/T) joint
2.38 Posterior view of the scapulothoracic (S/T) joint
2.39 A 3D view of the scapulothoracic joints
The sliding capability of the scapulothoracic joint is unique. While it is easy to envision the scapula sliding over ribs 2–7, in reality, it is the subscapularis sliding over the serratus anterior (2.40), as when you do a pushup (2.41). The scapula is capable of moving in multiple directions as it slides across the thoracic wall.
 2.40 Subscapularis and serratus anterior
2.40 Subscapularis and serratus anterior
2.41 Using the scapulothoracic joint for doing a pushup
The dynamic properties of the scapulothoracic joint are made possible by 17 muscles that either originate from or insert onto the scapula. If any one of them is dysfunctional, it can negatively impact the scapulohumeral rhythm, or the ratio of glenohumeral movement in relation to the scapulohumeral movement during arm elevation.
Of those 17 muscles, seven specifically provide dynamic support for the scapulothoracic joint. The most superficial of these muscles are the trapezius and the latissimus dorsi. The intermediate muscles are the levator scapulae, rhomboid minor, and rhomboid major. The deepest muscles bring us right back to the subscapularis and the serratus anterior. The remaining 10 muscles provide more of a static support system for the S/T joint (2.42, 2.43).
 2.42 Posterior view of muscles supporting the scapulothoracic joint
2.42 Posterior view of muscles supporting the scapulothoracic joint
 2.43 Anterior view of the muscles supporting the scapulothoracic joint
2.43 Anterior view of the muscles supporting the scapulothoracic joint
|
Dynamic Supporting Muscles |
Static Supporting Muscles |
|
Trapezius Latissimus dorsi Levator scapulae Rhomboid minor Rhomboid major Subscapularis Serratus anterior |
Supraspinatus Infraspinatus Teres minor Teres major Biceps brachii Long head of the triceps brachii Deltoid Coracobrachialis Pectoralis minor Omohyoid |
The following videos show each of the dynamic supporting muscles in 3D (2.44–2.50).
2.44 A 3D view of the trapezius muscles
2.45 A 3D view of the latissimus dorsi muscles
2.46 A 3D view of the levator scapulae muscles
2.47 A 3D view of the rhomboid minor muscles
2.48 A 3D view of the rhomboid major muscles
2.49 A 3D view of the subscapularis muscles
2.50 A 3D view of the serratus anterior muscles
Injury to the scapulothoracic joint is not very common. However, dysfunction related to this joint can be problematic for the shoulder complex—particularly for the glenohumeral joint—often resulting in biomechanical issues. Additionally, any dysfunction can potentially have detrimental effects on posture.
Let us look at one example of scapulothoracic dysfunction that you will no doubt see as a clinician: winging of the scapula (2.51). While there are many types of winging of the scapula, the most common of them involves the serratus anterior. If the serratus anterior is weak or neurologically (long thoracic nerve) impaired, it will have limitations in securing the medial border and anterior, inferior angle of the scapula in its proper position. What is its proper position? The serratus anterior holds the medial border/wall of the scapula against the thoracic cage (almost—remember, the bones do not actually touch). When the serratus anterior is weakened, it is unable to maintain the position of the scapula, resulting in a scapula that protrudes outward, looking like a wing.
2.51 Winging of the scapula is an example of scapulothoracic dysfunction.
Connecting the Dots
Can you think of any other muscles that, if weakened, may lead to winging of the scapula?
*Hint: Think about the origins and insertions of the muscles that act on the scapula.
Some examples:
Brain Builders: The Scapulothoracic Joint
[Students will use this quiz to review what they have learned.]
Bursae are incredibly important structures in any anatomical complex, and the shoulder is no exception. A bursa is a fluid-filled sac that provides protection for a soft tissue as it slides over a bony prominence by reducing the friction between the two structures.
What’s in a Name?
Bursa is the Latin word for purse.
Within the shoulder complex there are six bursae that warrant a deeper understanding (2.52).
2.52 Bursae within the shoulder complex
The supra-acromial bursa (2.53) has little notoriety because it is rarely injured. But it is worth noting its anatomical location, superior to the acromion. While injury is rare, the supra-acromial bursa does offer some protection for the trapezius and deltoid tendons. The trapezius—specifically, the middle trapezius—inserts into the acromion, and the deltoid originates from the acromion.
2.53 Supra-acromial bursa
Similar to the supra-acromial bursa, the coracoclavicular bursa (2.54) receives little attention, but it, too, is a relevant piece of the puzzle in the shoulder complex. The coracoclavicular bursa, also known as the supracoracoid bursa, is situated between the two components of the coracoclavicular ligament, the conoid and the trapezoid, acting as a buffer. The coracoclavicular is not a singular bursa but may consist of as many as three bursae.
2.54 Coracoclavicular bursa
The subacromial bursa is positioned in the subacromial space between the acromion and the supraspinatus tendon (2.55). The primary function of the subacromial bursa is to buffer the supraspinatus tendon as it runs beneath the acromion. If the tendon loses this protection, it will rub against the acromion and, eventually, the fibers of the supraspinatus tendon will fray and weaken the tendon. Potentially, this could result in a tear of the supraspinatus tendon (2.56). Due to its close proximity to the subacromial space, the infraspinatus tendon also benefits from the buffering role of the subacromial bursa.
2.55 Subacromial bursa
2.56 Torn supraspinatus tendon
The subdeltoid bursa (2.57) is an interesting piece of the shoulder complex puzzle. In many anatomy resources, it is considered a continuation of the subacromial bursa, making subacromial the largest bursa in the human body. However, the two bursae are not connected in the majority of humans. The subdeltoid bursa is inferior to the deltoid muscle and extends from the humeral head and greater tubercle to the deltoid tuberosity. It is fairly large, even independent of the subacromial bursa. Its size is notable, as it protects the deltoid muscle from the surfaces of the humerus, greater tubercle, and deltoid tuberosity.
2.57 Subdeltoid bursa
The subcoracoid bursa is located between the anterior surface of the subscapularis muscle and the coracoid process (2.58). The subcoracoid bursa acts as a buffer not only for the anterior subscapularis tendon but also for the tendons of the coracobrachialis and the short head of the biceps brachii. These tendons lie deep to the subcoracoid bursa.
2.58 Subcoracoid bursa
The subscapularis bursa is positioned between the subscapularis muscle and the scapula (2.59). This bursa is a flat and irregularly shaped structure, much like the scapula. The subscapularis bursa acts to cushion the subscapularis muscle against the anterior scapular wall.
2.59 Subscapularis bursa
Injury to a bursa typically occurs as a result of too much pressure or friction exerted over the fluid-filled sac. This increased friction causes irritation, and the bursa becomes swollen due to an increase and a thickening of the synovial fluid. This is referred to as bursitis. It can be acute or chronic. Acute bursitis occurs as a result of an unwelcomed, abrupt pressure, such as a direct blow to the area where the bursa is located. Chronic bursitis is also an unwelcomed traumatic event but it is insidious in nature; the pressure applied to the involved bursa occurs over time in a subtle and gradual manner, resulting in damage to the bursa.
While any of the bursae within the shoulder complex may be injured and become problematic, the best example of a bursa pathology is Secondary Impingement Syndrome (SIS). Simply described, SIS is a decrease in the subacromial space due to the swelling of any or all of the soft tissues running through it. These soft tissues include the long head of the biceps brachii tendon, the supraspinatus tendon, and the subacromial bursa. With a repetitive overhead activity, such as throwing a softball, the subacromial bursa may become impinged between the humeral head and/or supraspinatus tendon and the acromion (2.60). The result can be a very painful pinching feeling—ouch!
2.60 Subacromial impingement
The shoulder complex is truly that … complex. With so many pieces to this intriguing and intricate puzzle, it is worth the patience and time to piece it together (2.61).
2.61 The puzzle of the shoulder complex is complete!
Brain Builders: Bursae within the Shoulder Complex
[Students will use this quiz to review what they have learned.]
![]()
Just as the human body is linked together by the kinetic chain, let us link what we learned in Chapter 2. A good way to do that is to revisit the questions from the beginning of the chapter to inspire discussion with your peers and instructor. We can also link to current evidence to further explore the questions.
To link to generalized discussion points online, go to booksofdiscovery.com, “For Students.”
1. Both in middle-aged to older patients and in younger patients who participate in overhead activities, rotator cuff injuries are more common. Based upon the functional anatomy of the shoulder, which rotator cuff tendon is the most likely to be injured?
David C. Tapscott and Matthew Varacallo, “Supraspinatus Tendonitis,” StatPearls, updated August 4, 2023, https://www.ncbi.nlm.nih.gov/books/NBK551702/.
2. The shoulder complex has many bursae within it and each plays an important role for its proper function. What is the general role of a bursa in the human body?
Juliette R. Mercadante and Raghavendra Marappa-Ganeshan, “Anatomy, Skin Bursa,” StatPearls, updated October 8, 2022, https://www.ncbi.nlm.nih.gov/books/NBK554438/.
3. Over the past couple of decades, there has been an increase in shoulder injuries in fast-pitch softball pitchers. Can you speculate as to the reason(s) why?
Jeff Barfield and Gretchen Oliver, “What Do We Know about Youth Softball Pitching and Injury?” Sports Medicine - Open 4, no. 50 (November 19, 2018), https://sportsmedicine-open.springeropen.com/articles/10.1186/s40798-018-0168-6.
Abrams, Rachel, and Halleh Akbarnia. “Shoulder Dislocations Overview.” StatPearls. Updated August 8, 2023. https://www.ncbi.nlm.nih.gov/books/NBK459125/.
Aguirre, Kenneth, Andrew Mudreac, and John Kiel. “Anatomy, Shoulder and Upper Limb, Subscapularis Muscle.” StatPearls. Updated August 30, 2022. https://www.ncbi.nlm.nih.gov/books/NBK513344.
Arnander, Magnus, and Duncan Tennent. “Clinical Assessment of the Glenoid Labrum.” Shoulder Elbow 6, no. 4 (October 2014): 291–99. https://pubmed.ncbi.nlm.nih.gov/27582948/.
Barfield, Jeff, and Gretchen Oliver. “What Do We Know about Youth Softball Pitching and Injury?” Sports Medicine - Open 4, no. 50 (November 19, 2018). https://doi.org/10.1186/s40798-018-0168-6.
Biel, Andrew. Trail Guide to the Body: A Hands-On Guide to Locating Muscles, Bones, and More. 6th ed. Boulder, CO: Books of Discovery, 2019.
Burkart, Andreas C., and Richard E. Debski. “Anatomy and Function of the Glenohumeral Ligaments in Anterior Shoulder Instability.” Clinical Orthopaedics and Related Research 400 (July 2002): 32–39. https://pubmed.ncbi.nlm.nih.gov/12072743/.
Chang, Lou-Ren, Prashanth Anand, and Matthew Varacallo. “Anatomy, Shoulder and Upper Limb, Glenohumeral Joint.” StatPearls. Updated August 8, 2022. https://www.ncbi.nlm.nih.gov/books/NBK537018/.
Colas, F., J. Nevoux, and O. Gagey. “The Subscapular and Subcoracoid Bursae: Descriptive and Functional Anatomy.” Journal of Shoulder and Elbow Surgery 13, no. 4 (July 2004): 454–58. https://www.jshoulderelbow.org/article/S1058-2746(04)00047-3/ppt.
Druel, Thibault, Marius Buffard, Laurent Nové-Josserand, and Arnaud Walch. “Role of Middle Glenohumeral Ligament in External Shoulder Rotation.” JSES International 7, no. 2 (March 2023): 331–35. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9998722/.
Frank, Rachel M., Jose Ramirez, Peter N. Chalmers, Frank M. McCormick, and Anthony A. Romeo. “Scapulothoracic Anatomy and Snapping Scapula Syndrome.” Anatomy Research International (November 28, 2013). https://pubmed.ncbi.nlm.nih.gov/24369502/.
Gong, Ji-Cheng, Na Chen, Jia-Fei Chen, Zhou Xu, Yi Wu, Jin-Qing Li, and Kang-Lai Tang. “Subscapular Bursa: Anatomy and Magnetic Resonance Appearance.” Chinese Medical Journal (English) 130, no. 14 (July 20, 2017): 1739–40. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5520564/.
Jeno, Susan H., Akul Munjal, and Gary S. Schindler. “Anatomy, Shoulder and Upper Limb, Arm Supraspinatus Muscle.” StatPearls. Updated August 30, 2022. https://www.ncbi.nlm.nih.gov/books/NBK537202.
Klatte-Schulz, Franka, Kathi Thiele, Markus Scheibel, Georg N. Duda, and Britt Wildemann. “Subacromial Bursa: A Neglected Tissue Is Gaining More and More Attention in Clinical and Experimental Research.” Cells 11, no. 4 (February 14, 2022): 663. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8870132/.
Lam, Joshua H., and Bruno Bordoni. “Anatomy, Shoulder and Upper Limb, Arm Abductor Muscles.” StatPearls. Updated August 30, 2022. https://www.ncbi.nlm.nih.gov/books/NBK537148.
Mercadante, Juliette R., and Raghavendra Marappa-Ganeshan. “Anatomy, Skin Bursa.” StatPearls. Updated October 8, 2022. https://www.ncbi.nlm.nih.gov/books/NBK554438/.
Morell, Daniel J., and David S. Thyagarajan. “Sternoclavicular Joint Dislocation and Its Management: A Review of the Literature.” World Journal of Orthopedics 7, no. 4 (April 18, 2016): 244–50. https://www.wjgnet.com/2218-5836/full/v7/i4/244.htm.
Rothenberg, Adam, Gregory Gasbarro, Jesse Chlebeck, and Albert Lin. “The Coracoacromial Ligament: Anatomy, Function, and Clinical Significance.” Orthopaedic Journal of Sports Medicine 5, no. 4 (April 27, 2017). https://pubmed.ncbi.nlm.nih.gov/28508008/.
Sambandam, Senthil Nathan, Vishesh Khanna, Arif Gul, and Varatharaj Mounasamy. “Rotator Cuff Tears: An Evidence Based Approach.” World Journal of Orthopedics 6, no. 11 (December 18, 2015): 902–18. https://pubmed.ncbi.nlm.nih.gov/26716086/.
Tapscott, David C., and Matthew Varacallo. “Supraspinatus Tendonitis.” StatPearls. Updated August 4, 2023. https://www.ncbi.nlm.nih.gov/books/NBK551702/.
Varacallo, Matthew, and Scott D. Mair. “Proximal Biceps Tendinitis and Tendinopathy.” StatPearls. Updated September 4, 2022. https://www.ncbi.nlm.nih.gov/books/NBK533002.
Williams, Jestin M., Margaret A. Sinkler, and William Obremskey. “Anatomy, Shoulder and Upper Limb, Infraspinatus Muscle.” StatPearls. Updated August 8, 2022. https://www.ncbi.nlm.nih.gov/books/NBK513255.
Yi, Min, Fan Yang, Jingjing An, and Fuguo Huang. “Effect of Glenohumeral Ligaments on Posterior Shoulder Stabilization: A Biomechanical Study.” American Journal of Translational Research 15, no. 3 (March 15, 2023): 1953–63. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10086893/.
Zhao, Jinlong, Minghui Luo, Guihong Liang, Ming Wu, Jianke Pan, Ling-Feng Zeng, Weiyi Yang, and Jun Liu. “Risk Factors for Supraspinatus Tears: A Meta-analysis of Observational Studies.” Orthopaedic Journal of Sports Medicine 9, no. 10 (October 12, 2021). https://pubmed.ncbi.nlm.nih.gov/34660827/.
Hyperlinked key terms
[in order of appearance in the chapter]
chronic – injury that occurs over time and is a result of overuse
capsulitis – inflammation of the joint capsule resulting in stiffness and tightness of the joint
kinetic chain – a movement pattern’s predictable sequence through a series of interrelated links or segments; movement of one segment will impact the movement pattern at the proximal and distal segments
biomechanics – the study of forces acting on and generated within a body and the effects of these forces on the various tissues within the body
turf toe – a sprain of the first metatarsophalangeal joint, usually as a result of hyperextension of the big toe
congruency – the amount of surface area between two bones in contact with one another
acute – a sudden and spontaneous trauma resulting from a specific and identifiable event; such an event often involves high-intensity forces and is of short duration
sagittal plane – a vertical plane that separates the body into left and right segments
transverse plane – a horizontal plane that separates the body into superior and inferior segments
frontal plane – a vertical plane that separates the body into anterior and posterior segments
oblique plane – a plane that is neither horizontal nor vertical, separating the body at an angle and involving two or more of the cardinal planes (sagittal, frontal, and transverse); most human movement occurs in an oblique plane
synovial – a joint that is freely mobile and has a joint cavity; the most common type of joint in the body
fibrocartilaginous – having dense, white connective tissue with a fibrous texture; examples include intervertebral discs, meniscus, labrum
axial skeleton – the core portion of the bony skeleton, consisting of 80 bones that make up the head, neck, and trunk
proprioception – the unconscious or conscious awareness of the body in space; the use of joint position sense and joint motion sense to respond to stresses placed upon the body by alteration of posture and movement (your “sixth sense”)
mechanoreceptors – sensory receptors that detect changes in tension, pressure, stretch, and motion
mechanism of injury – the method(s) by which damage occurs to connective tissue, muscle tissue, and the nervous system
separated shoulder – the incongruency of the clavicle and acromion, where the clavicle moves superiorly away from the acromion as a result of a damaged acromioclavicular ligament and, potentially, the coracoclavicular ligament
critical shoulder angle (CSA) – angle formed between the glenoid and the most lateral border of the acromion process
concentrically – actively shortening
eccentrically – actively lengthening
scapulohumeral rhythm – the ratio of glenohumeral movement in relation to the scapulohumeral movement during arm elevation, typically 2:1. For every 2° of motion occurring with the humerus (flexion and abduction), the scapula moves 1° of motion (upward rotation).
winging of the scapula – a failure of the dynamic stabilizers of the scapula, leading to an altered position of the scapula
bursa – a fluid-filled sac that reduces the friction between two structures
bursitis – swelling or inflammation of a bursa
pathology – the structural and functional changes due to disease, including its causes, origins, and natures
Daniel J. Morell and David S. Thyagarajan, “Sternoclavicular Joint Dislocation and Its Management: A Review of the Literature,” World Journal of Orthopedics 7, no. 4 (April 18, 2016): 244–50, https://www.wjgnet.com/2218-5836/full/v7/i4/244.htm. ↑
Morell and Thyagarajan, “Sternoclavicular Joint Dislocation and Its Management.” ↑
Andreas C. Burkart and Richard E. Debski, “Anatomy and Function of the Glenohumeral Ligaments in Anterior Shoulder Instability,” Clinical Orthopaedics and Related Research 400 (July 2002): 32–39, https://pubmed.ncbi.nlm.nih.gov/12072743/; Thibault Druel et al., “Role of Middle Glenohumeral Ligament in External Shoulder Rotation,” JSES International 7, no. 2 (March 2023): 331–35, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9998722/; Min Yi et al., “Effect of Glenohumeral Ligaments on Posterior Shoulder Stabilization: A Biomechanical Study,” American Journal of Translational Research 15, no. 3 (March 15, 2023): 1953–63, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10086893/. ↑
Jinlong Zhao et al., “Risk Factors for Supraspinatus Tears: A Meta-analysis of Observational Studies,” Orthopaedic Journal of Sports Medicine 9, no. 10 (October 12, 2021), https://pubmed.ncbi.nlm.nih.gov/34660827/. ↑
Rachel Abrams and Halleh Akbarnia, “Shoulder Dislocations Overview,” StatPearls, updated August 8, 2023, https://www.ncbi.nlm.nih.gov/books/NBK459125/. ↑
Abrams and Akbarnia, “Shoulder Dislocations Overview.” ↑